
Steve Shaha
Institute for Integrated Outcomes, USA
Title: Analytics lead to significant improvements clinical and cost outcomes for patients, clinicians and care organizations
Biography
Biography: Steve Shaha
Abstract
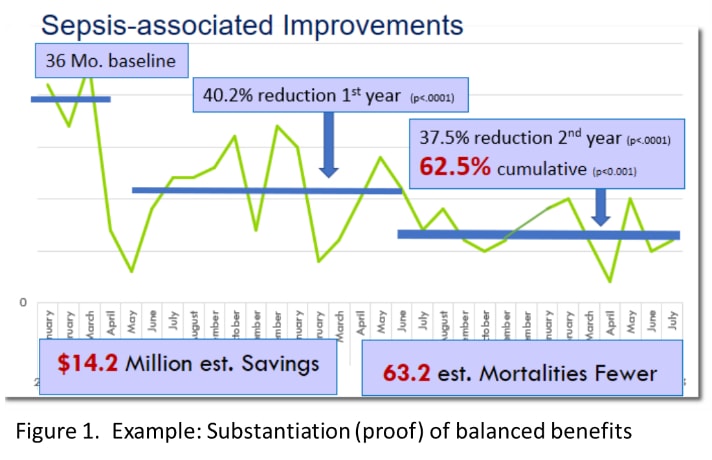
Electronic patient records (EPRs) have proliferated throughout global healthcare. Too often however, and for too many care organizations, the objective is mostly about maximise financial performance blindly of clinical impacts, particularly within healthcare models dependent upon viability of privately owned healthcare organisations. Regardless, proof of well-balanced benefits to clinical outcomes, cost reductions and user satisfaction remain unjustifiably rare. In healthcare, this lack of substantiation is arguably unconscionable.
The mission and purpose of healthcare and organisations remains improved care to restore or enhance the health and wellbeing of persons and populations. This mission is beyond records computerisation alone, and the mission of computerisation must represent a match in purpose. At its foundational level the mission is only accomplished by pairing the most appropriate clinicians, with patients matched with needs, all within the most clinically appropriate and cost-effective delivery setting. Translated to modern healthcare, that care-giver, recipient and setting match ideally represents the most cost-effective, readily accessible and clinically delivering model. Therefore the mission of computerisation must reflect those needs, and be justified by the benefits required for all.
A vast collection has been amassed reflecting substantive, quantified and compelling gains – proof – in benefits reflecting the needed balance of clinical, cost, satisfaction and efficiency improvements. Case studies shared substantiate improvements in the full array of benefits needed, including improved Sepsis occurrence and care, Transfusion rates, Medication errors (adult and Paediatric), Stroke care and outcomes, Obstetric care and infant complications/mortalities, Cardiology and reduced in-house arrests, Thrombolytics, Orthopedics, Pulmonology, Urology, IV to PO (oral) medication conversions, and beside caregiver inclusive efficacy. Also, maximised benefits for telehealthcare, community integration, emergency utilization, hospitalizations, length of stay, and others. Sharing these examples will provide sufficient background for analogous success throughout healthcare organisations and models.
Recent Publications:
- Adams, H. P., Del Zoppo, G., Alberts, M. J., Bhatt, D. L., Brass, L., Furlan, A., & Wijdicks, E. F. (2007). Guidelines for the Early Management of Adults With Ischemic Stroke. Circulation, 115(20).
- Audebert, H. J., Kukla, C., von Claranau, S. C., Kühn, J., Vatankhah, B., Schenkel, J., & Horn, M. (2005). Telemedicine for Safe and Extended Use of Thrombolysis in Stroke The Telemedic Pilot Project for Integrative Stroke Care (TEMPiS) in Bavaria. Stroke, 36(2).
- Bates, D. W. (2002). The quality case for information technology in healthcare. BMC Medical Informatics and Decision Making, 2(1).
- Fichman, R. G., Kohli, R., & Krishnan, R. (Eds.). (2011). Editorial overview-the role of information systems in healthcare: Current research and future trends. Information Systems Research, 22(3).
- Hick, J. L., Hanfling, D., Burstein, J. L., DeAtley, C., Barbisch, D., Bogdan, G. M., & Cantrill, S. (2004). Health care facility and community strategies for patient care surge capacity. Annals of Emergency Medicine, 44(3).

